Incisional Hernia Repair
- GI & Bariatric Surgery
- Whipple Surgery
- Bariatric Surgery
- Liver Resection
- Gastro Esophageal Surgeries
- Colorectal Surgeries
- Appendectomy
- Hemorrhoidectomy
- Partial Colectomy
- Nissen Fundoplication
- Piles Surgery
- Peptic / Gastric Ulcer Treatment
- Gastrointestinal Surgery
- Surgery for Morbid Obesity
- Hepatopancreaticobiliary Surgery
- Post-Cholecystectomy Bile Duct Injury
- Incisional Hernia
- Minimally Invasive Surgery
- Gallbladder (Biliary) Stone Treatment
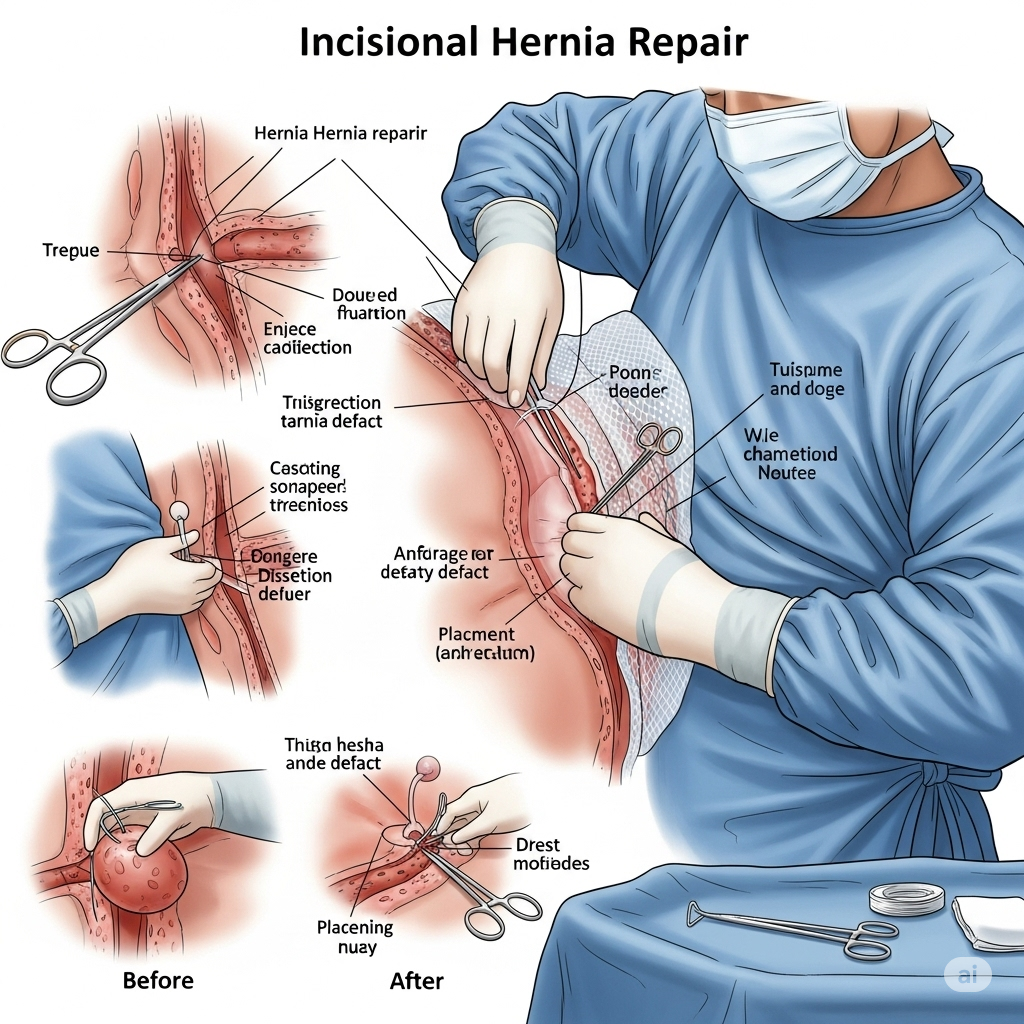
Incisional Hernia Repair
Incisional Hernia: Expert Management and Repair
**Incisional Hernia** is a type of hernia that occurs at or near the site of a previous surgical incision in the abdominal wall. It happens when the surgical wound fails to heal completely, allowing abdominal contents (like intestines or fat) to push through the weakened muscle and fascia, forming a bulge. While the surgical repair of an incisional hernia is performed by a general surgeon, **Dr. Neeraj Dhar, a leading Gastroenterologist in Faridabad, plays an important supportive role** in the comprehensive care of patients, particularly in **pre-operative gastrointestinal optimization and post-operative management of any related digestive issues.**
Understanding Incisional Hernias and Their Causes:
Any abdominal surgery can potentially lead to an incisional hernia, as the incision weakens the abdominal wall. Factors that increase the risk include:
- **Wound Infection:** Impairs healing.
- **Excessive Strain:** Coughing, vomiting, heavy lifting, or straining during bowel movements after surgery.
- **Obesity:** Places increased pressure on the abdominal wall.
- **Poor Nutrition:** Affects tissue healing.
- **Certain Medical Conditions:** Such as diabetes, chronic lung disease (leading to chronic cough), or conditions that weaken connective tissue.
- **Steroid Use.**
- **Large or Multiple Incisions.**
Symptoms of Incisional Hernia:
- **Visible Bulge:** A soft lump or swelling at or near the surgical scar, especially noticeable when standing, coughing, or straining.
- **Pain or Discomfort:** Often worse with physical activity.
- **Nausea or Vomiting:** If the bowel becomes trapped (incarcerated).
- **Constipation or Changes in Bowel Habits.**
- **Redness or Tenderness:** Indicating potential complications like incarceration or strangulation (when blood supply to the trapped tissue is cut off, a surgical emergency).
Diagnosis:
Diagnosis typically involves:
- **Physical Examination:** The surgeon can usually identify the hernia by feeling the bulge.
- **Imaging Studies:** Ultrasound, CT scan, or MRI may be used to confirm the diagnosis, assess the size of the hernia, identify its contents (e.g., bowel, omentum), and check for any complications.
When is Surgery Indicated?
Surgical repair is generally recommended for incisional hernias that are:
- **Symptomatic:** Causing pain or discomfort.
- **Progressively Enlarging:** Growing in size.
- **Irreducible:** Cannot be pushed back into the abdomen.
- **Risk of Complications:** Such as incarceration (trapped bowel) or strangulation (blood supply cut off, a medical emergency requiring immediate surgery).
Types of Incisional Hernia Repair:
The choice of surgical technique depends on the hernia's size, location, and the patient's overall health:
1. Open Hernia Repair:
- The surgeon makes a single incision over the hernia site.
- The protruding tissue is pushed back into the abdominal cavity.
- The weakened abdominal wall is then repaired, often by suturing the muscles together and reinforcing the area with a synthetic mesh.
- **Mesh Repair:** Most common, providing strong support and reducing recurrence rates.
2. Laparoscopic Hernia Repair (Minimally Invasive):
- Several small incisions are made away from the hernia site.
- A laparoscope (a thin tube with a camera) and specialized instruments are inserted.
- The hernia contents are pushed back, and a mesh is typically placed on the inside of the abdominal wall.
- **Benefits:** Smaller incisions, less pain, shorter hospital stay, faster recovery.
3. Robotic-Assisted Hernia Repair:
- A variation of laparoscopic surgery where the surgeon controls robotic arms to perform the repair.
- Offers enhanced precision, dexterity, and 3D visualization, particularly beneficial for complex or recurrent hernias.
Preparation for Surgery:
As a Gastroenterologist, Dr. Neeraj Dhar's pre-operative assessment can be crucial:
- **General Health Optimization:** Managing underlying conditions like diabetes, hypertension, and respiratory issues.
- **Bowel Preparation:** For very large hernias, or if there's a risk of bowel involvement, specific bowel preparation might be needed.
- **Weight Management:** If obesity is a factor, weight loss may be recommended before surgery to reduce recurrence risk.
- **Smoking Cessation:** To improve wound healing.
- **Gastrointestinal Assessment (by Dr. Neeraj Dhar):** Evaluation for chronic constipation, inflammatory bowel disease, or severe GERD (which can cause chronic coughing) that could increase abdominal pressure and affect surgical outcomes or recurrence risk. Addressing these conditions pre-operatively helps ensure a smoother recovery.
Recovery and Post-Operative Care:
- **Pain Management:** Pain medication will be prescribed.
- **Activity Restrictions:** Avoiding heavy lifting, straining, and strenuous activities for several weeks to allow the repair to heal.
- **Wound Care:** Instructions on keeping the incision site clean and dry.
- **Diet:** A normal diet can usually be resumed once tolerated. Dr. Dhar can provide guidance on maintaining healthy bowel function post-surgery to prevent straining.
- **Follow-up:** Regular follow-up appointments with the surgeon and, if GI issues arise, with Dr. Neeraj Dhar.
Potential Risks and Complications:
While generally safe, incisional hernia repair carries potential risks:
- **Recurrence:** The hernia can come back, especially if risk factors are not addressed or for very large hernias.
- **Pain:** Acute post-operative pain, or sometimes chronic pain (especially with mesh).
- **Infection:** Of the wound or the mesh (if used).
- **Bleeding or Hematoma (blood collection).**
- **Seroma (fluid collection).**
- **Damage to surrounding organs:** Such as the bowel or nerves.
- **Adhesions:** Scar tissue formation.
- **Anesthesia risks.**
Dr. Neeraj Dhar's Contribution to Incisional Hernia Care:
Though not performing the surgery, Dr. Neeraj Dhar's gastroenterological expertise enhances overall patient care for incisional hernias:
- **Pre-operative GI Optimization:** He assesses and manages any underlying gastrointestinal conditions that could impact the surgical outcome or increase the risk of hernia recurrence. This includes addressing chronic constipation, irritable bowel syndrome, inflammatory bowel disease, or severe gastroesophageal reflux disease (GERD) causing chronic cough, which puts strain on the abdominal wall.
- **Nutritional Assessment:** Ensuring patients are in optimal nutritional status to support wound healing, especially critical for larger or complex hernias.
- **Post-operative Bowel Management:** He provides guidance on diet and medication to ensure regular, soft bowel movements, minimizing straining that can put pressure on the surgical repair.
- **Management of Post-operative GI Complications:** If patients experience new or exacerbated digestive issues after surgery (e.g., severe constipation, bloating, changes in bowel habits), Dr. Dhar can diagnose and manage these effectively, ensuring a smoother overall recovery.
- **Risk Factor Management:** He helps identify and manage GI-related risk factors that might contribute to hernia development or recurrence, such as chronic intra-abdominal pressure.
If you have an incisional hernia or are preparing for its repair, a comprehensive approach involving both a skilled surgeon and a gastroenterologist like Dr. Neeraj Dhar in Faridabad can ensure optimal health and recovery. Consult with him for expert pre-operative assessment and post-operative GI care.
